This Mom Donated Her Lost Baby’s Tissue to Research
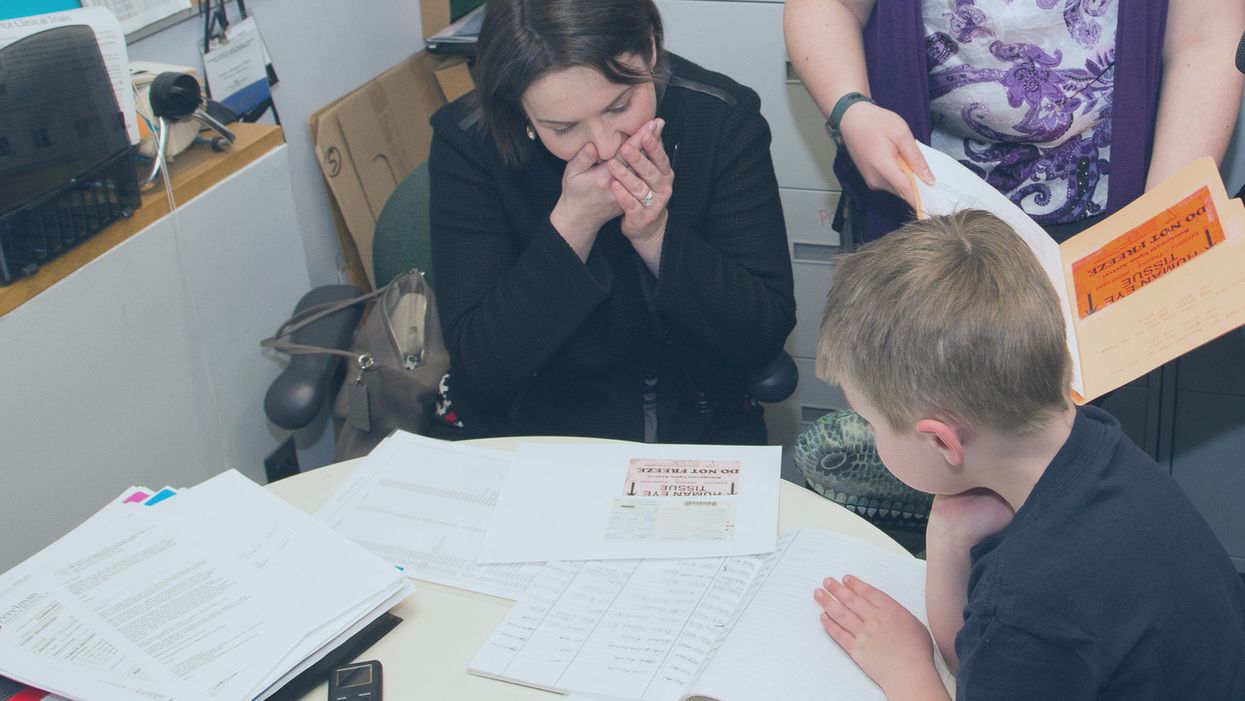
Sarah Gray views data about the use of her deceased son Thomas' retinal tissue in research for retinoblastoma, a cancer of the eye, at the University of Pennsylvania, while her son Callum looks on.
The twin boys growing within her womb filled Sarah Gray with both awe and dread. The sonogram showed that one, Callum, seemed to be the healthy child she and husband Ross had long sought; the other, Thomas, had anencephaly, a fatal developmental disorder of the skull and brain that likely would limit his life to hours. The options were to carry the boys to term or terminate both.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.
Sarah learned that researchers prize tissue as essential to better understanding and eventually treating the rare disorder that afflicted her son. And that other tissue from the developing infant might prove useful for transplant or basic research.
Animal models have been useful in figuring out some of the basics of genetics and how the body responds to disease. But a mouse is not a man. The new tools of precision medicine that measure gene expression, proteins and metabolites – the various chemical products and signals that fluctuate in health and illness – are most relevant when studying human tissue directly rather than in animals.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.

Thomas Gray
(Photo credit: Mark Walpole)
Later Sarah would track down where some of the donated tissues had been sent and how they were being used. It was a rare initiative that just may spark a new kind of relationship between donor families and researchers who use human tissue.
Organ donation for transplant gets all the attention. That process is simple, direct, life saving, the stories are easy to understand and play out regularly in the media. Reimbursement fully covers costs.
Tissue donation for research is murkier. Seldom is there a direct one-to-one correlation between individual donation and discovery; often hundreds, sometimes thousands of samples are needed to tease out the basic mechanisms of a disease, even more to develop a treatment or cure. The research process can be agonizingly slow. And somebody has to pay for collecting, processing, and getting donations into the hands of appropriate researchers. That story rarely is told, so most people are not even aware it is possible, let alone vital to research.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care.
The dichotomy between transplant and research became real for Sarah several months after the birth of her twins, and Thomas' brief life, at a meeting for families of transplant donors. Many of the participants had found closure to their grieving through contact with grateful recipients of a heart, liver, or kidney who had gained a new lease on life. But there was no similar process for those who donated for research. Sarah felt a bit, well, jealous. She wanted that type of connection too.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care. Those encounters were as novel for the researchers as they were for Sarah. The experience turned her into an advocate for public education and financial and operational changes to put tissue donation for research on par with donations for transplant.
Thomas' retina had been collected and processed by the National Disease Research Interchange (NDRI), a nonprofit that performs such services for researchers on a cost recovery basis with support from the National Institutes of Health. The tissue was passed on to Arupa Ganguly, who is studying retinoblastoma, a cancer of the eye, at the University of Pennsylvania.
Ganguly was surprised and apprehensive months later when NDRI emailed her saying the mother of donated tissue wanted to learn more about how the retina was being used. That was unusual because research donations generally are anonymous.
The geneticist waited a day or two, then wrote an explanation of her work and forwarded it back through NDRI. Soon the researcher and mother were talking by phone and Sarah would visit the lab. Even then, Ganguly felt very uncomfortable. "Something very bad happened to your son Thomas but it was a benefit for me, so I'm feeling very bad," she told Sarah.
"And Sarah said, Arupa, you were the only ones who wanted his retinas. If you didn't request them, they would be buried in the ground. It gives me a sense of fulfillment to know that they were of some use," Ganguly recalls. And her apprehension melted away. The two became friends and have visited several times.

Sarah Gray visits Dr. Arupa Ganguly at the University of Pennsylvania's Genetic Diagnostic Laboratory.
(Photo credit: Daniel Burke)
Reading Sarah Gray's story led Gregory Grossman to reach out to the young mother and to create Hope and Healing, a program that brings donors and researchers together. Grossman is director of research programs at Eversight, a large network of eye banks that stretches from the Midwest to the East Coast. It supplies tissue for transplant and ocular research.
"Research seems a cold and distant thing," Grossman says, "we need to educate the general public on the importance and need for tissue donations for research, which can help us better understand disease and find treatments."
"Our own internal culture needs to be shifted too," he adds. "Researchers and surgeons can forget that these are precious gifts, they're not a commodity, they're not manufactured. Without people's generosity this doesn't exist."
The initial Hope and Healing meetings between researchers and donor families have gone well and Grossman hopes to increase them to three a year with support from the Lions Club. He sees it as a crucial element in trying to reverse the decline in ocular donations even while research needs continue to grow.
What people hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
Since writing about her experience in the 2016 book "A Life Everlasting," Gray has come to believe that potential donor families, and even people who administer donation programs, often are unaware of the possibility of donating for research.
And roadblocks are common for those who seek to do so. Just like her, many families have had to be persistent in their quest to donate, and even educate their medical providers. But Sarah believes the internet is facilitating creation of a grassroots movement of empowered donors who are pushing procurement systems to be more responsive to their desires to donate for research. A lot of it comes through anecdote, stories, and people asking, if they have done it in Virginia, or Ohio, why can't we do it here?

Callum Gray and Dr. Arupa Ganguly hug during his family's visit to the lab.
(Photo credit: Daniel Burke)
Gray has spoken at medical and research facilities and at conferences. Some researchers are curious to have contact with the families of donors, but she believes the research system fosters the belief that "you don't want to open that can of worms." And lurking in the background may be a fear of liability issues somehow arising.
"I believe that 99 percent of what happens in research is very positive, and those stories would come out if the connections could be made," says Sarah Gray. But what they hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.
Urinary tract infections account for more than 8 million trips to the doctor each year.
Few things are more painful than a urinary tract infection (UTI). Common in men and women, these infections account for more than 8 million trips to the doctor each year and can cause an array of uncomfortable symptoms, from a burning feeling during urination to fever, vomiting, and chills. For an unlucky few, UTIs can be chronic—meaning that, despite treatment, they just keep coming back.
But new research, presented at the European Association of Urology (EAU) Congress in Paris this week, brings some hope to people who suffer from UTIs.
Clinicians from the Royal Berkshire Hospital presented the results of a long-term, nine-year clinical trial where 89 men and women who suffered from recurrent UTIs were given an oral vaccine called MV140, designed to prevent the infections. Every day for three months, the participants were given two sprays of the vaccine (flavored to taste like pineapple) and then followed over the course of nine years. Clinicians analyzed medical records and asked the study participants about symptoms to check whether any experienced UTIs or had any adverse reactions from taking the vaccine.
The results showed that across nine years, 48 of the participants (about 54%) remained completely infection-free. On average, the study participants remained infection free for 54.7 months—four and a half years.
“While we need to be pragmatic, this vaccine is a potential breakthrough in preventing UTIs and could offer a safe and effective alternative to conventional treatments,” said Gernot Bonita, Professor of Urology at the Alta Bro Medical Centre for Urology in Switzerland, who is also the EAU Chairman of Guidelines on Urological Infections.
The news comes as a relief not only for people who suffer chronic UTIs, but also to doctors who have seen an uptick in antibiotic-resistant UTIs in the past several years. Because UTIs usually require antibiotics, patients run the risk of developing a resistance to the antibiotics, making infections more difficult to treat. A preventative vaccine could mean less infections, less antibiotics, and less drug resistance overall.
“Many of our participants told us that having the vaccine restored their quality of life,” said Dr. Bob Yang, Consultant Urologist at the Royal Berkshire NHS Foundation Trust, who helped lead the research. “While we’re yet to look at the effect of this vaccine in different patient groups, this follow-up data suggests it could be a game-changer for UTI prevention if it’s offered widely, reducing the need for antibiotic treatments.”

